This briefing note forms part of our wider study into the outsourcing of NHS eye care services to the private sector.
Read MoreThis briefing note forms part of our wider study into the outsourcing of NHS eye care services to the private sector.
Read MoreThis report analyses the contractual mechanisms of NHSE’s £2bn+ deal with the private hospital sector during COVID, building on our 2021 report ‘For Whose Benefit’ using newly obtained activity data and the contracts themselves.
Read MoreThis report presents the views of England’s Directors of Public Health on the latest reforms to public health.
Read MoreA two year study examining the financial impacts of the pandemic on UK care homes for older people and their staff.
Read MoreThis report analyses the government’s use of the private hospital sector to alleviate the burden on the NHS during the first year of the COVID pandemic.
Read MoreThis analysis maps the network of joint venture businesses between NHS medical consultants and private healthcare companies.
Read MoreThis report finds that reforms made to the NHS following the Health and Social Care Act of 2012 have impacted upon its ability to deal effectively with a possible flu pandemic.
Read MoreThis report looks into how the private hospital sector uses financial incentives to attract NHS consultants to work for them.
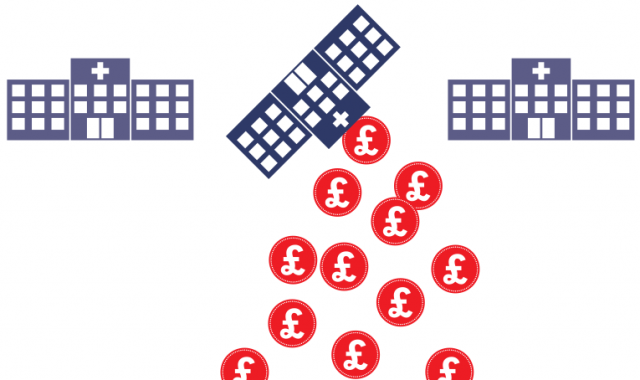
Read MoreThis report analyses the financing structure of the new Private Finance 2 scheme and finds that it is likely to increase costs to the NHS. Restructuring the balance of debt and risk capital would increase the rate of return to private investors by 15% compared to the original Private Finance Initiative.
Read MoreThis report analyses five options available to policy makers to address the problems caused by existing PFI schemes.
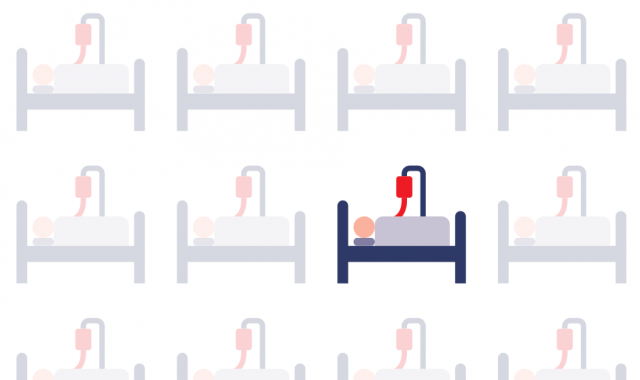
Read MoreBased on evidence from an extensive review of CQC inspection reports of 177 private hospitals in England, this report identifies serious risks to patient safety in the current private hospital business model.
Read MoreThis report brings together what is known about patient safety in private hospitals. It offers new insights into the number of patient safety incidents in private hospitals, analyses the potential risks inherent in the way that these services operate, and makes recommendations to improve transparency in the private sector.
Read MoreThis report identifies where each pound that goes into the care home industry ends up by using a forensic study of the accounts of over 830 adult care home companies. If finds significant levels of leakage of money from front-line care, including to profit, rental bills and debt repayments.
Read MoreThis report uses findings from the Care Quality Commission’s new inspection regime for private hospitals to show that there continue to be risks to patient safety associated with the distinctive nature of private hospitals in England, compared with the NHS.
Read MoreIn this report, we look at the less-than-expected growth in NHS treatment of private patients since the 2012 Health and Social Care Act, and consider whether the practice has been an effective means of generating additional revenues, and how it might impact on the availability of care for NHS patients.
Read MoreThis report looks at the significant profits made by PFI companies from NHS contracts over the last 6 years.
Read MoreThis report raises questions about the capacity of the NHS to handle the increasing outsourcing of its services to the private sector and its ability to ensure that services provided by the private sector under contract with the NHS are safe, effective and value for money.
Read MoreThis report warns that the introduction of greater use of for profit providers of healthcare services as a result of the 2012 Health and Social Care Act is likely to substantially increase the amount of healthcare fraud in the NHS.
Read MoreThis report looks at how the market in social care services in England provides the best available example for policy makers of what happens to the quality of care and the terms and conditions of the care workforce when competitive pressures are used to bring about a reduction in the cost of care to the taxpayer.
Read MoreThis report describes the role that privatisation has played in the decline of the provision and quality of adult social care. It outlines a number of reforms which could help reverse the decline in the sector.
Read More