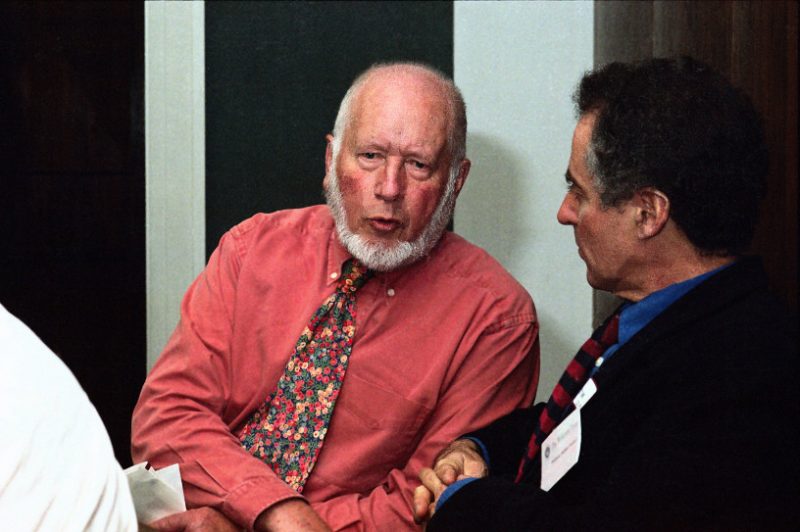
Photo Credit: Wellcome Library, Creative Commons by-nc 2.0 UK
Essays in honour of Julian Tudor Hart
Julian Tudor Hart was one of the most influential and inspirational doctors of the 20th century. He was a general practitioner who began his career shortly after the birth of the NHS and died aged 91 on 1 July 2018. Most of his working life was spent as a GP serving a very deprived mining community at Glyncorrwg in the Welsh valleys. Here he was able to combine research with his training in public health and the everyday care of his patients. He was able to study the effects of planned, anticipatory care over several decades. He understood that effective primary care depends on a solid foundation of trust and continuity.
This is the first of three essays looking at what Tudor Hart’s research and practice can teach us about contemporary primary care challenges, especially with regard to healthcare inequalities and to technological innovations that support and improve care, and those which disrupt it.
Prior to the 1970s and 80s, GPs opened their doors in the morning and waited for patients to come in. Patients went to the doctor because they felt sick. Doctors did not, on the whole, call patients in to check their blood pressure or monitor their diabetes, they were busy enough trying to meet the demands of those already suffering. Tudor Hart remembered seeing up to 300 patients a day for barely 2-3 minutes each, which was clearly barely adequate for addressing their immediate concerns, never mind any health promotion or prevention.
Determined to combine the treatment of symptomatic disease with prevention, he began by systematically identifying people at risk and proactively treating their blood pressure and addressing their risk factors. As a result, he reduced mortality by 50% over 25 years.((Julian Tudor Hart et al., ‘Twenty Five Years of Case Finding and Audit in a Socially Deprived Community’, BMJ 22 June 1991))) Four key lessons stand out from his work.
1. Start with evidence.
By the 1970s, research had shown that high blood pressure, smoking, uncontrolled diabetes, obesity and (later) raised cholesterol were all risk factors for heart disease, including fatal heart attacks. There were effective treatments for blood pressure and diabetes, and patients could be helped to stop smoking, and potentially to lose weight and reduce cholesterol, by modifying their diet. These were proven interventions that weren’t reaching the people who could benefit from them.
2. Identify unmet need.
It was known that there was a ‘rule of halves’ whereby only half of those at risk had been identified and of those, only half were on treatment, and of those on treatment, only half were adequately treated.((Julian Tudor Hart, A New Kind of Doctor, London, The Merlin Press 1988, pages 109-115)) Tudor Hart had to find a way to identify everyone registered with his practice who was at risk and monitor their care. He needed better record-keeping and recall systems, and computers seemed ideally suited to assist with this. The process of converting the old paper notes into computerized records took an estimated 1300 hours of staff time. Completing the process by 1989, his was one of the first practices to use electronic patients’ records. They managed to screen 98% of the practice population for blood pressure, mainly by opportunistic checks when patients came in for other problems, then by call up and finally by home visits.
3. Make sure you have the necessary resources.
Thirteen hundred hours of staff time is an enormous commitment. Tudor Hart wrote that ‘it took many years and much work to meet high demands well enough to make space for innovation. Whole-population care through organised case finding and audit is feasible but only with a labour-intensive approach combining accessibility, flexibility, and continuity, as well as a planned and structured approach, which requires substantial expansion of staff numbers and assiduous recording.’
4. Technology, evidence and resources aren’t enough. You need a solid base of trusting, human relationships.
Like Tudor Hart I am a GP in a deprived area where it is very hard to persuade patients to come in for routine reviews when they are living insecure lives overwhelmed by chronic pain, anxiety and depression and quite often living in fear of destitution and/or violence. For these patients, consultations need to be long enough to combine the alleviation of suffering, which is ‘the natural and necessary priority for sick people [and] is the basis for credibility of doctors and nurses to the public’, with the prevention of disease. Tudor Hart continued:
‘Most of our measurements were obtained during consultations prompted by patient demand, and we generally found that this is the best way to approach working class patients. This view and its converse (that working-class people at high-risk respond poorly to health promotion clinics) have been generally endorsed by others.
‘The health authority seemed unable to understand that staff continuity was essential for high compliance in a working-class population.’
Lessons for today
1. Technology should support relationship-based primary care, not disrupt it. Tudor Hart introduced electronic patient records to ensure that the unmet needs of the most vulnerable patients could be met. Yet today ‘disruptive’ innovation is being promoted as a good thing even though the evidence shows that it rarely succeeds((https://bjgp.org/content/bjgp/67/660/320.full.pdf)), and when it also disrupts the way care is provided the most able are the first to benefit and the most vulnerable are the last. This has been the case with GP At Hand, a partnership between a health app developer, Babylon, and a GP practice, that allows consultation via a mobile phone app but has no capacity for providing care for patients with long term conditions. We’ll look at this more closely in the next essay.
2. If you want to innovate you must be able to meet demand. Calls for innovation in the NHS are coming at a time of unprecedented funding cuts where the needs of patients who are suffering, especially those with long-term mental health conditions, are not being met. Like very many GPs I am having to work extra clinical sessions every week and haven’t been able to devote time to anything innovative (like group consultations) for months.
3. Innovations should be based on evidence. Proven interventions to prevent the complications and early deaths that result from hypertension, diabetes, smoking and obesity are still not reaching those who need them most, while we are being forced to spend time on things that have not been shown to be effective, like telehealth and digital triage. We need to focus on what we already know to be effective and do it better.
4. Continuity of care still matters. Trust in health professionals and the NHS remains exceptionally high but is being undermined by public criticism by politicians and the media. For vulnerable patients, whose ability to trust authority may have been undermined repeatedly in early life, trust is earned through long-term relationships with people who care for and about them. There is no way to short-cut this. For suggestions of what policy makers and clinicians can do about it, there is an essay here.
It is almost impossible to talk about blood pressure to someone who has just been sanctioned because they failed their benefits assessment, but Julian Tudor Hart proved that if you gain the trust of your patients and work with them for years, guided by evidence, you can combine care with prevention and reduce suffering and premature death.
Support Our Work
CHPI is the only truly independent health think-tank dedicated to the founding principles of the NHS. To continue our work keeping the public interest at the centre of health and social care policy, we need your help.
Please support CHPI so we can continue to impact the health policy debate.
